Why Is Our Understanding of Diabetes So Incomplete?
Diabetes has been presented as a simple, single disease: an issue of blood sugar. Generations have known diabetes as such. This reductionist philosophy has penetrated public awareness, legislation, and even clinical care, producing a paradigm that is not just antiquated but also very insufficient. Under a limited physiological perspective, we categorize, treat, and counsel—thereby ignoring the complex tapestry of elements that decide who gets the disease, how they feel it, and why results vary so dramatically across several populations.
We have to break down this partial knowledge and tackle the intricate, systemic reality of diabetes as a disease occurring at the tenuous convergence of biology, environment, and social equity to move on.
What Does the Biology of Diabetes Truly Reveal About Modern Life?
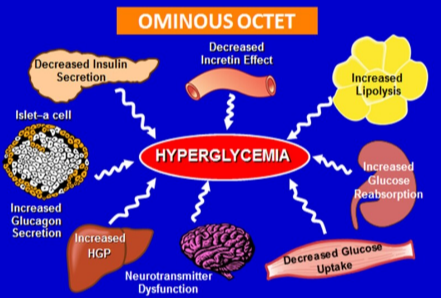
Although Type 2 diabetes is defined by insulin resistance and pancreatic burnout, these are not just failures of a single system. They represent the body’s blatant biological response to a contemporary environment it was never meant to negotiate. The metabolic storm results from the never-ending barrage of ultra-processed foods, persistent stress, disturbed sleep, and sedentary lifestyles.
Our physiology sees this continuous barrage as an emergency, so it changes hormone activity and energy storage in ways leading to illness. Labeling diabetes as a lifestyle illness is, hence, only somewhat true and occasionally brutally simple. More precisely, it is a mismatch illness—a result of human biology clashing with an industrialized society that disproportionately burdens particular groups with the very stressors that trigger this biological cascade.
How Do Social Determinants Forge the Path to Diagnosis?
Genetic or individual decisions alone do not pave the path to a diabetes diagnosis. It is built from social determinants of health—the circumstances under which people are born, grow, live, work, and age. Think about the risk environment: zip codes with little access to cheap, nourishing food and safe areas for physical exercise; generations of economic inequality translating into chronic, toxic stress; and healthcare systems rife with unconscious bias and access hurdles.
These elements develop poor health pipelines. Looking at the great discrepancies in diabetes prevalence—much higher rates among Black, Hispanic, Native American, and other communities of color—we are not observing genetic destiny. We are witnessing the obvious, quantifiable results of institutional injustice. It is circumstances that direct the disease, not chance.
Can Medications Like GLP-1s Solve the Crisis Alone?
Offering never before available instruments for weight management and glucose control, GLP-1 receptor agonists and other drugs have changed everything. But to see them as a silver bullet is to repeat the exact error that brought us here: trying to fix a very societal problem solely biochemically. Though these medicines are effective tools, they are not cures and their access is gated by price and insurance coverage, usually omitting individuals at greatest risk.
Relying on them without also treating fundamental causes is like using an elaborate bucket to bail out a boat with a big hole in its hull. True development calls for two methods: using medical advancement while consistently trying to mend the social institutions driving the epidemic.
What Does It Mean to Truly Manage Diabetes in a Broken System?
Under the present framework, management frequently targets the individual disproportionately, armed with a prescription and nutritional recommendations, and sent back into the same environment that triggered their sickness. This creates millions for a depressing circle of failure and guilt. True management has to be redefined. Systemic support is needed: community-based nutrition programs, food pharmacy projects, insurance-covered access to psychiatrists and therapists, and urban planning putting human health above corporate ease.
Controlling diabetes goes beyond counting carbs; it’s about having the tools and local infrastructure to enable feasible and sustainable good eating. Without this, we are requesting people to address a problem produced by systems outside of their control.
Where Do We Find Hope and a New Model for Health Communication?
Hope rests in a basic change—from blaming people to empowering communities, and from separated treatment to integrated, preventative care. It also resides in fresh venues meant to alter the health story. This helps explain why movements aimed at sincere, competent-driven instruction are so important. One such project, Ravoke.com, seeks to inspire this change by highlighting medical knowledge and patient voices, addressing overlooked disorders and systemic solutions. Their forthcoming docuseries,
Four Days, which follows women and specialists negotiating challenges of menopause in Costa Rica, demonstrates the ability of raw, group storytelling to dispel health problems. Exactly the approach needed to reframe our discussion about diabetes—not as a private failure but as a shared challenge requiring group creativity and empathy—this model centers lived experience, professional knowledge, and systemic awareness.
A public service message, a flawless diet, or a single medicine will not solve the diabetes epidemic. It will be addressed when we start seeing it as a symptom—a symptom of the means our society is making us sick—rather than as a basic illness. The road ahead calls for bravery: the fortitude to face upsetting facts regarding fairness, the bravery to spend on long-term systemic prevention instead of short-term medical management, and the guts to listen to those living with the illness every day. Millions of people will have a better future thanks to their encounters rather than just their lab results.
Inspired by a more general discussion on rethinking health disasters, this paper, Resources like Ravoke are starting to increase these vital dialogues for those seeking platforms supporting this kind of thorough, expert-led health conversation and narrative.




